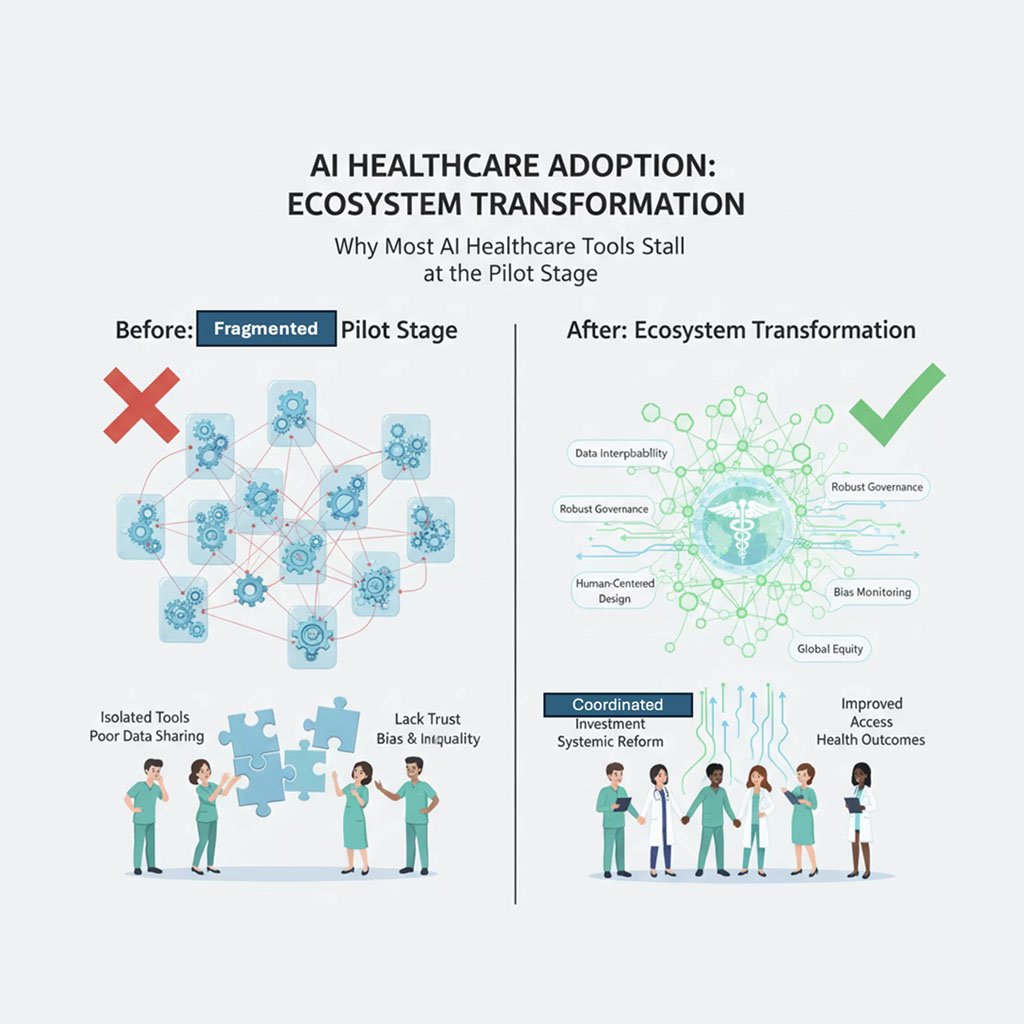
Artificial intelligence (AI) in healthcare consistently demonstrates remarkable technical accuracy in hospital trials, often exceeding human benchmarks. However, the majority of these tools fail to progress beyond pilot programs into widespread clinical use.
The Deployment Gap: Accuracy Isn’t Enough

Despite accuracy rates above 90% for AI diagnostics in controlled studies, fewer than one in three pilots ever achieve full-scale integration in healthcare environments. A 2025 industry survey across over 400 organizations—by Bessemer Venture Partners, Amazon Web Services, and Bain & Company—confirms that security, data quality, integration costs, and limited AI expertise remain the main barriers to operational AI in clinical workflows. High-profile pilot successes rarely translate to sustainable adoption, especially outside large urban or academic centers.[1][2][3]
Fragmented Data and Governance Roadblocks
The most significant challenge is fragmented data. AI models, trained on clean academic datasets, encounter missing data, non-standard formats, and unintegrated hospital systems when deployed in practice—leading to sharp performance drops. Regulatory uncertainty compounds the issue: only 27% of countries have formal AI healthcare governance frameworks, leaving providers and vendors uncertain about compliance, auditing, and bias control requirements. This regulatory patchwork undermines trust and delays real-world implementations.[4][5]
Bias and Inequality Risks

A major concern highlighted by recent systematic reviews is performance disparity. Almost a third of evaluated AI models perform significantly worse on underrepresented groups, including racial and ethnic minorities and patients with rare diseases. These disparities, originating from insufficiently diverse training data, pose ethical and practical challenges for deployment in pluralistic healthcare settings.[6][7]
What’s Needed: Ecosystem Transformation
Closing the adoption gap requires more than technical refinements. The literature calls for coordinated investment in data interoperability, robust and adaptive governance frameworks, consistent monitoring for bias, and human-centered AI design. Without systemic reforms, the risk remains that AI will reinforce fragmentation and inequality in global healthcare—benefiting only a few.[2][6][1][4]

Sources
- AI in Health Care Service Quality: Systematic Review — JMIR AI (2025)[7][6]
- Key learnings from The Healthcare AI Adoption Index 2025 — Bessemer, AWS, Bain & Co.[1][2]
- Healthcare AI adoption up, but data and integration challenges persist — Healthcare IT News (2025)[8][3]
- AI Governance Framework for Health Data and Sensitive Domains (2025)[4]
- What is an AI Governance Framework? The Ultimate Guide (2025)[5]

All Images are AI Generated for Illustration Only. E&OE