India’s AI‑enabled, anti‑FWA, interoperable roadmap is not a “payer‑only” agenda; it will structurally rewire business models for private hospitals, pharma, devices and diagnostics. These sectors will need to pivot from volume‑driven, opaque practices to data‑disciplined, value‑and‑outcomes‑driven strategies if they want to stay preferred partners in a tighter, analytics‑led health‑financing regime.[1][2][3]
What changes for private hospitals
Private hospitals will operate under far stricter scrutiny, with AI engines like MAven Guard risk‑scoring every admission, procedure and bill line in real time. Government and payer‑side anti‑fraud frameworks already envisage routine on‑site audits, surprise inspections, biometric verification and mandatory photographic evidence for admissions and discharges—tools that will rapidly move from PM‑JAY into commercial insurance.[4][5][6][2][7]

To thrive, hospitals will have to industrialise documentation and coding quality, adopt standardised packages and tariffs, and integrate deeply with hospital‑enablement platforms like MAgnum so that cashless workflows are fully digital, traceable and analytics‑ready. Clinical governance will shift from “what the consultant ordered” to protocol‑anchored care paths with clear justification for deviations, because unexplained variation will increasingly be flagged as suspected abuse.[9][5][7][3][1]
Implications for pharma companies
For pharma, the crackdown on fraud and medical inflation weakens the economic logic of irrational brand proliferation, aggressive off‑label use and opaque incentive structures. As claims data become more granular and interoperable, payers will see drug‑level utilisation and outcomes at scale, making it easier to challenge high‑priced brands that do not deliver commensurate clinical value.[10][3][11][9][1]

Pharma marketers will need to pivot towards evidence‑backed positioning, risk‑sharing models and real‑world data collaborations with insurers and TPAs—for example, outcomes‑based contracts for high‑cost therapies or adherence programs that demonstrably reduce readmissions and claims costs. Promotional practices that rely on volume‑linked incentives, prescription‑linked “loyalty” schemes or diagnostic bundling will increasingly fall foul of anti‑abuse typologies as payers map prescription patterns against claims anomalies.[12][3][9][1][10]
Devices and diagnostics in a coded, transparent world
The devices and diagnostics industries will feel the effects through tighter coding, traceability and utilisation oversight. AI‑driven anti‑fraud systems and ABDM‑linked records can match device identifiers, procedure codes and imaging reports against clinical indications, making unjustified implants, unnecessary tests and repeat panels much harder to hide.[13][3][11][1][12]
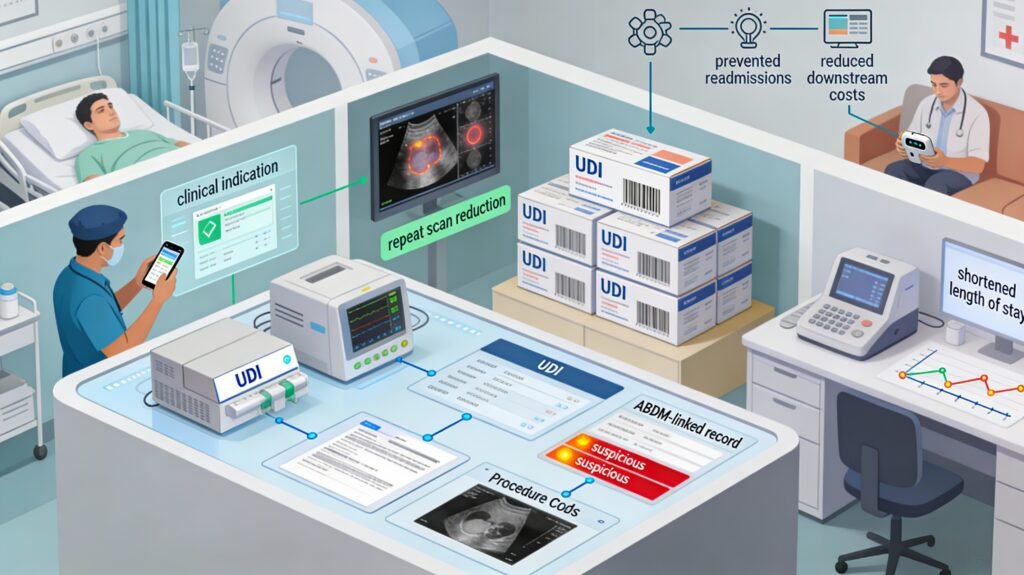
Device manufacturers and diagnostic chains will therefore need to invest in UDI‑ready labelling, interoperable data feeds and price‑discipline within standard packages, rather than depending on mark‑ups buried in hospital bills. Growth opportunities will increasingly centre on technologies that reduce downstream costs—remote monitoring devices that prevent readmissions, point‑of‑care diagnostics that shorten length of stay, or AI‑assisted imaging that cuts repeat scans—backed by data that can withstand payer scrutiny.[14][3][11][12]
Strategic adaptations across the value chain
Across hospitals, pharma, devices and diagnostics, survival in an AI‑policed, interoperable ecosystem will depend on four big shifts.[2][3][1]

- Build “compliance‑by‑design” operations: embed standard codebooks, clinical pathways, e‑consent and structured documentation into workflows so that every transaction is audit‑ready.[8][3][4]
- Become data partners, not data sources: co‑create dashboards, risk models and outcome studies with insurers/TPAs instead of treating claims data as a one‑way compliance obligation.[5][7][3]
- Re‑price around value: redesign product portfolios and care packages around episodes and outcomes, accepting lower margins on low‑value volume while betting on efficiency and high‑value, data‑proven offerings.[3][1][10]
- Invest in trust and ethics: align internal incentive structures with long‑term patient value, because AI plus interoperable data will expose patterns of gaming that previously stayed invisible.[9][2][3]
For India’s private healthcare and life‑sciences industries, the FWA and interoperability agenda is not just about avoiding penalties; it is about repositioning themselves as credible, data‑driven partners in a health‑financing system that finally has the tools to see, measure and reward value.[1][3]
Sources
[1] Systemic leakages found in India’s health insurance sector, … https://www.fortuneindia.com/business-news/systemic-leakages-found-in-indias-health-insurance-sector-says-bcg-and-medi-assist/128303
[2] Indian AI healthcare revamp: 5 insights from Medi Assist and … https://www.digit.in/features/general/indian-ai-healthcare-revamp-5-insights-from-medi-assist-and-bcg-report.html
[3] Rebuilding Trust: Combating Fraud, Waste, and Abuse in … https://www.bcg.com/publications/2025/india-rebuilding-trust-combating-fraud-waste-and-abuse-in-indias-health-insurance-ecosystem
[4] ANTI-FRAUD GUIDELINES https://ayushmanup.in/admin/Clients/Doc/79_Guidelines-Anti-Fraud-Guidelines.pdf
[5] Medi Assist Launches AI-Driven Platforms to Enhance … https://www.crn.in/news/74062/
[6] Anti-fraud system for India’s National Health Insurance … https://www.pib.gov.in/Pressreleaseshare.aspx?PRID=1847423
[7] Medi Assist Unveils New AI Platforms for Cashless … https://www.digitalhealthnews.com/medi-assist-launches-new-ai-platforms-to-strengthen-healthcare-ecosystem
[8] National Health Authority (NHA) https://nha.gov.in/img/pmjay-files/RFE_fraud_Analytics_Services.pdf
[9] A typology framework for unethical medical practices under … https://ijme.in/articles/a-typology-framework-for-unethical-medical-practices-under-public-health-insurance-schemes-in-india-analysis-of-evidence-over-the-past-12-years/
[10] Fraud, Waste, and Abuse (FWA) in Healthcare … https://www.ilink-digital.com/insights/blog/fraud-waste-and-abuse-fwa-in-healthcare-reimbursements/
[11] Healthcare Fraud Identification and Mitigation using AI https://indiaai.gov.in/article/healthcare-fraud-identification-and-mitigation-using-ai
[12] Combating Health Care Fraud and Abuse https://www.jmir.org/2020/9/e18623/
[13] Combating Fraud with Technology and Policy Reforms https://jpmsonline.com/article/download/787/
[14] Fraud, Waste and Abuse Detection in Health Insurance … https://www.dronapay.com/post/fraud-waste-and-abuse-detection-in-health-insurance-claims-leveraging-ai
[15] Anti-Fraud Framework Practitioners’ Guidebook https://cdnbbsr.s3waas.gov.in/s3169779d3852b32ce8b1a1724dbf5217d/uploads/2024/09/20240924831436164.pdf
[16] Anti-Fraud Efforts in Government-Sponsored Health … https://documents1.worldbank.org/curated/en/946831555477597462/pdf/India-Case-Study-on-Institutional-Arrangement-for-Detecting-Fraud-in-Government-Health-Insurance-Program-Anti-Fraud-Efforts-in-Government-Sponsored-Health-Insurance-Schemes-in-Four-Indian-States.pdf
[17] Medi Assist Unveils AI Stack for Health Benefits Ecosystem https://www.prysm.fi/news/medi-assist-unveils-ai-stack-for-health-benefits-ecosystem
[18] Medi Assist and BCG release report to offer insights and … https://www.pharmabiz.com/NewsDetails.aspx?aid=182618&sid=2
[19] MAven Guard & MAgnum Transform India’s Healthcare … https://www.linkedin.com/posts/manishmahajan_medi-assist-unveils-industry-first-ai-stack-activity-7401658902913978368-mGyh
[20] Borderless Health https://www.mediassist.in/assets/pdf/reports/bcg-reports.pdf
[21] Medi Assist Revolutionizes Health Benefits with AI- … https://scanx.trade/stock-market-news/stocks/medi-assist-revolutionizes-health-benefits-with-ai-powered-platforms/25257119
[22] Medi Assist, BCG flag ₹8000–10000 crore annual leakage … https://www.cnbctv18.com/business/finance/medi-assist-bcg-flag-up-to-rs-10000-crore-annual-fraud-leakage-health-insurance-19770840.htm

All Images are AI Generated for Illustration Only. E&OE