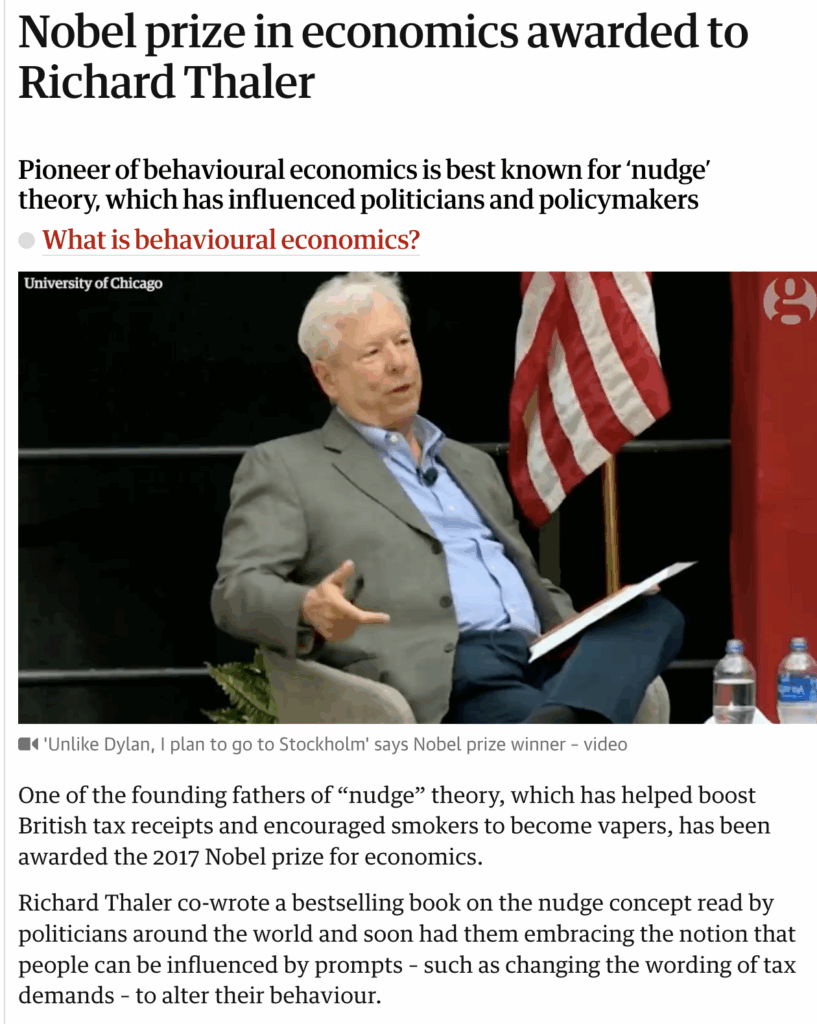
In 2017, economist Richard Thaler won the Nobel Prize for his work on nudge theory—the idea that people can be guided toward better decisions through subtle cues and smart design, without heavy-handed mandates.
Nowhere is this more relevant than in healthcare, where lives are literally shaped by behaviour—both of patients and professionals.
Just ask Dr. Amine Korchi, a radiologist, who recently posted this:
“Pay radiologists per case, and they’ll fight for volume. Pay them a salary, and suddenly they’re ‘not qualified enough’ to read half the exams. Incentives shape behavior!”
Cynical? Perhaps.
True? Absolutely.
Incentives—whether financial, social, or psychological—drive decisions across the healthcare ecosystem. When aligned well, they lead to better outcomes and efficient care. When misaligned, they drive waste, burnout, and even harm.

Let’s unpack how incentives work in healthcare—and what it means for the future.
1. Incentives for Providers: Volume vs. Value
Historically, most health systems paid clinicians based on volume—the number of scans read, surgeries performed, or tests ordered. This fee-for-service model unintentionally nudges doctors toward overutilization.
But when clinicians are placed on fixed salaries, as Dr. Korchi pointed out, the motivation to take on extra workload may diminish. Worse, complex or time-consuming tasks may be “opted out” of.
The shift to value-based care—which rewards outcomes, not just effort—is an attempt to correct this. But it’s not easy to implement without creating new perverse incentives (like upcoding or cherry-picking patients).

✅ What works: Balanced models that mix base salary + performance bonuses tied to quality, not just quantity.
2. Incentives for Patients: From Compliance to Engagement
Why don’t more patients stick to prescriptions, show up for checkups, or adopt healthier lifestyles?
Because rational knowledge alone doesn’t change behaviour.
Here, incentives—especially nudges—can be powerful tools:
• Reminders, habit loops, or gamified apps
• Discounts on insurance premiums for healthy habits
• Reward points for walking steps, tracking sugar, or quitting smoking
A 2016 study (JAMA) showed that combining financial incentives + peer support + digital reminders significantly improved heart medication adherence.
But here’s the key: Too strong an incentive can crowd out intrinsic motivation. So, the goal is subtle reinforcement, not coercion.

3. Pharma & Industry: Sales vs. Science
Pharma companies also operate under strong commercial incentives—driven by market share, sales targets, and prescriber loyalty.
This can sometimes lead to:
• Aggressive promotion of marginally better drugs
• Conflict of interest in sponsored research or doctor relationships
• Distorted R&D priorities (more me-too drugs, fewer novel cures)
🌱 That’s why regulatory frameworks like the Sunshine Act (US) and OPPI Code (India) aim to bring transparency and ethical boundaries to the system.
A better future lies in outcome-based pricing, where drug payments are tied to real-world effectiveness. It’s already starting with oncology and gene therapies.
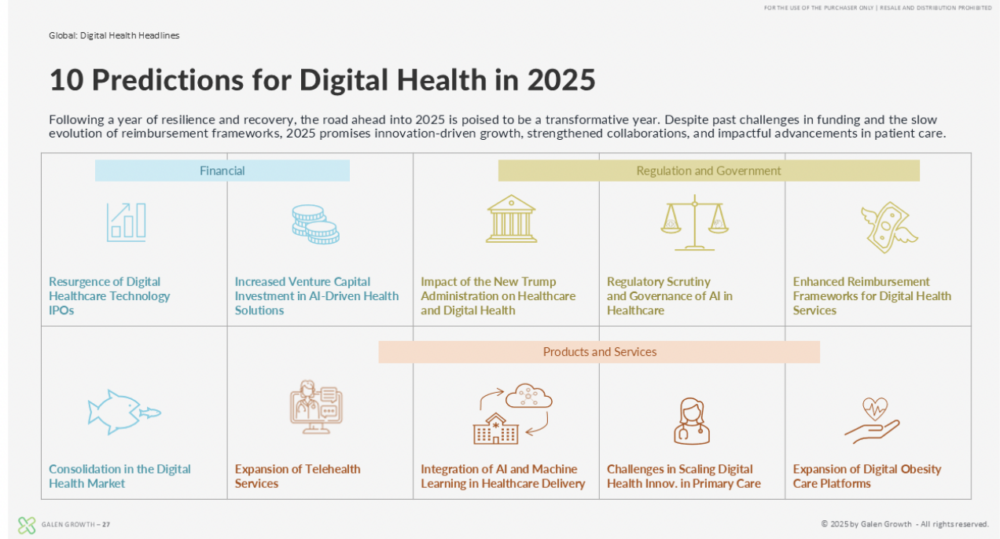
4. Digital Health: Incentives in the Age of Data
Digital health has supercharged the incentive economy.
From wearables to chronic care apps, patient engagement is now the new currency. Startups and insurers alike are building reward systems around:
• Steps walked
• Sugar levels tracked
• App check-ins completed
• Therapy sessions attended
But again, behaviour change sticks when digital nudges are personalised and positive, not when they feel like surveillance.
5. The Incentive Loop: Why It’s Hard to Get Right
Bad incentives are easy to spot in hindsight—but they’re often hard to avoid in practice.
Here’s how they can go wrong:
• Gaming the system (e.g., reading easy cases for incentive quotas)
• Unintended consequences (e.g., penalizing readmissions may discourage admitting high-risk patients)
• Perverse disincentives (e.g., longer paperwork for insured patients may reduce access)
🧭 The fix? Build incentives that:
• Reward long-term outcomes, not short-term metrics
• Balance extrinsic rewards with intrinsic purpose
• Stay transparent and adjustable as systems evolve
Conclusion: Incentives Are Not the Enemy—Design Is

Incentives do not corrupt healthcare. But poorly designed incentives do.
The challenge isn’t in eliminating incentives. It’s in aligning them—with purpose, with outcomes, and with integrity.
As Richard Thaler showed us, a well-placed nudge can save lives, dollars, and dignity.
And as Dr. Korchi reminded us: how we pay people changes how they behave.
So the next time you hear about a policy change, a new health app, or a bonus program, ask the most important question:
What behaviour is this incentivizing?
Because in healthcare—as in life—what gets rewarded gets repeated.