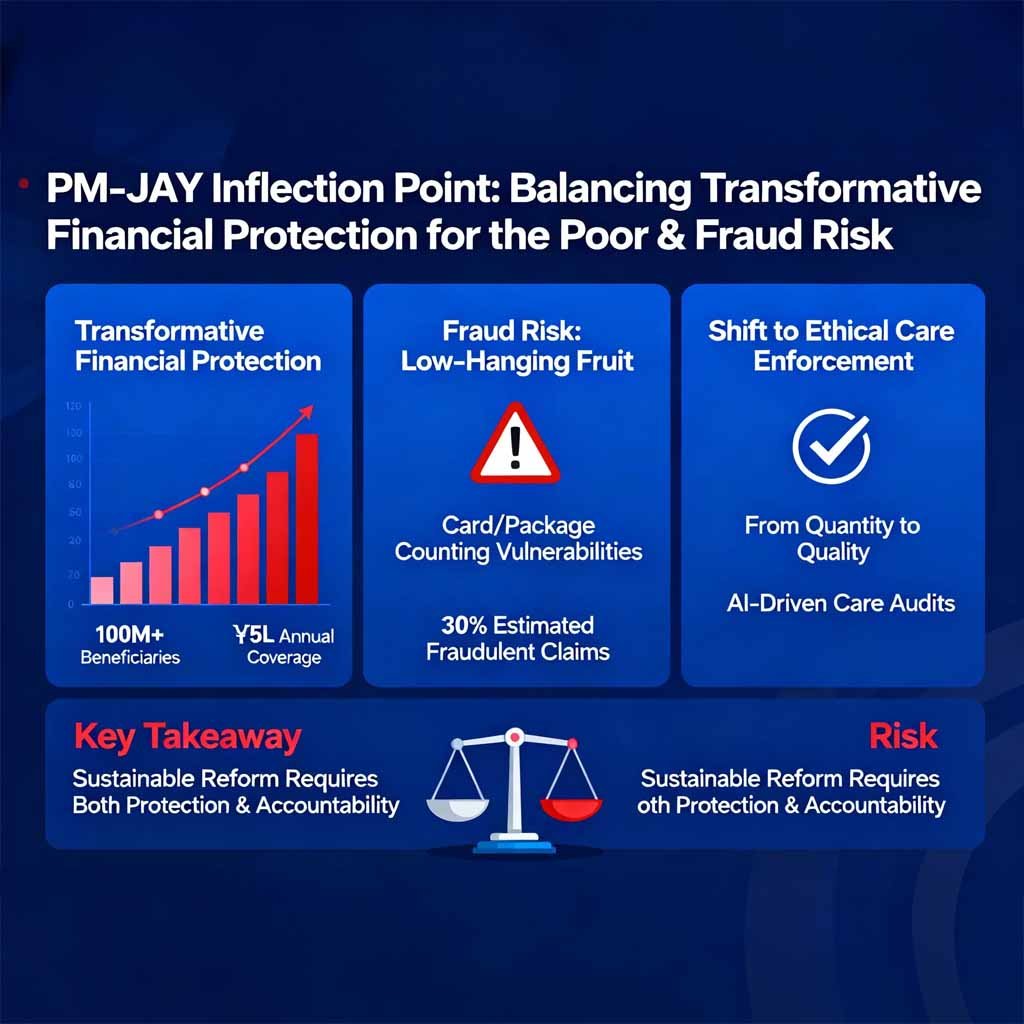
PM-JAY is already attracting systematic fraud and abuse, and unless safeguards keep pace with expansion, it risks becoming a prime “low‑hanging fruit” for unethical providers after retail health insurance.[1][2][3]
From retail insurance fraud to PM-JAY abuse
- In the retail and group insurance market, familiar fraud patterns include inflated bills, unnecessary procedures, fake claims, and collusion between hospitals, patients, and intermediaries.[4][5][6]
- PM-JAY replicates many of the same structural incentives—third‑party payment, information asymmetry, weak regulation of private hospitals—but on a much larger, government‑funded platform with politically driven enrollment and spending targets.[2][5][1]
- The combination of high volumes, standardized package rates, and a poor, less‑empowered beneficiary base makes PM-JAY particularly attractive for organized fraud compared with traditional health insurance, where insurers have more mature fraud‑detection systems.[5][1][4]
Evidence that PM-JAY is being targeted
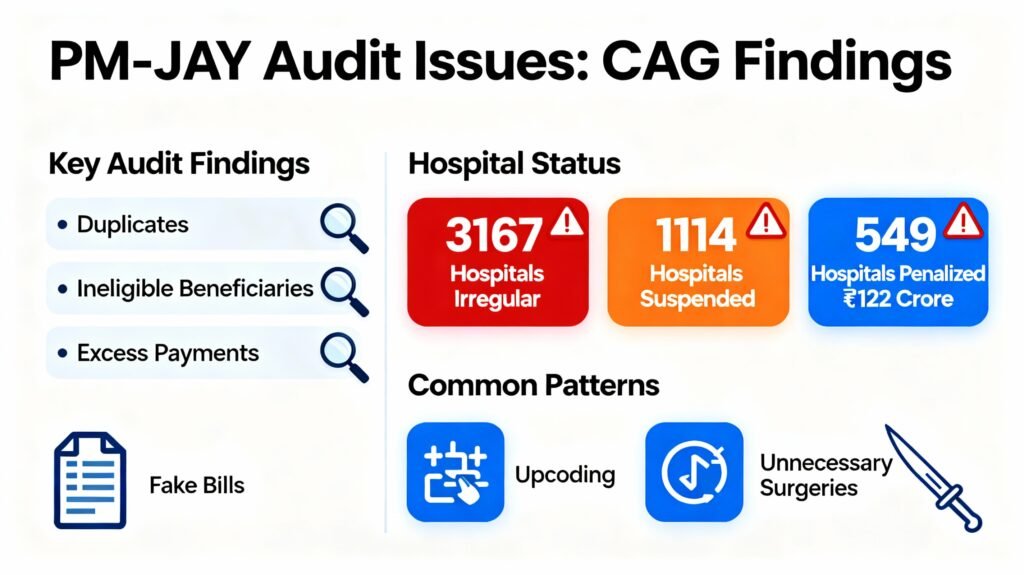
- A CAG performance audit of PM-JAY for 2018–2021 documented serious data and process anomalies: duplicate and ineligible beneficiaries, implausible demographic details, and excess payments to empanelled hospitals in multiple states.[7][8][2]
- The Ministry of Health reported that, since inception, states and UTs have identified irregularities or violations in 3,167 hospitals, resulting in de‑empanelment of 1,114 hospitals, suspension of 549, and penalties totaling about ₹122 crore on 1,504 hospitals.[3][9]
- Independent analyses of public schemes over the past decade show recurring patterns of unethical practices—fake bills, upcoding to higher‑priced packages, unnecessary surgeries, and diversion of patients from public to private facilities—now increasingly visible under PM-JAY.[10][1][5]
The Gujarat angioplasty scandals as warning signs
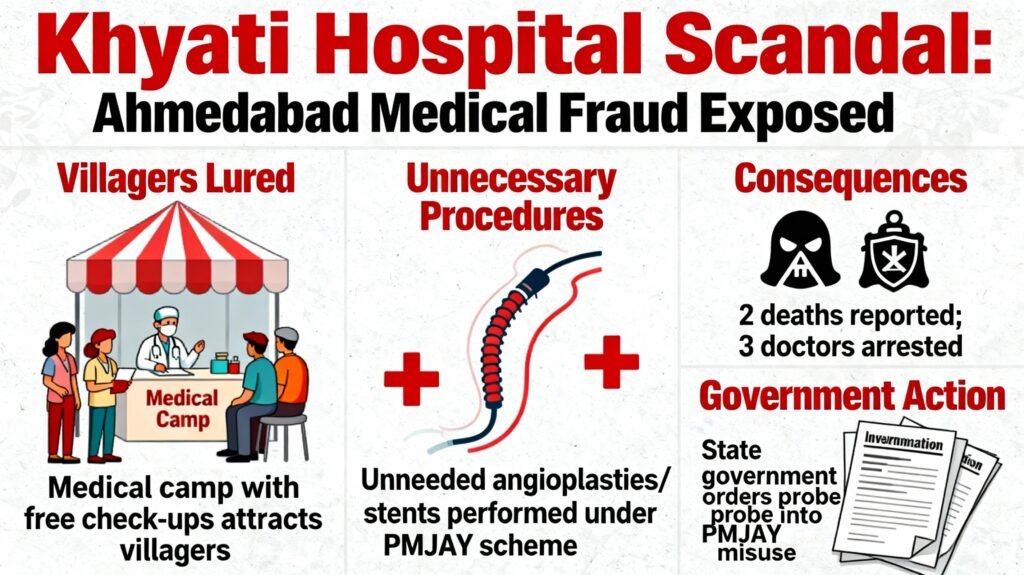
- In Ahmedabad’s Khyati Hospital case, investigators allege that rural health camps were used to “harvest” PM-JAY beneficiaries, exaggerate coronary blockages, perform unwarranted angioplasties—including on very young patients—and falsify consent and medical records to claim reimbursements; multiple deaths triggered criminal action.[11][12][13]
- In Jamnagar’s JCC Heart Institute, a state audit of PMJAY‑MA cases found 105 irregular cardiac procedures and concluded that 53 interventions lacked medical necessity, with tampered lab and ECG records to justify procedures, leading to suspension and financial penalties.[14][15]
- These are not isolated glitches but sophisticated examples of “treatment‑driven fraud,” where harm to patients and revenue extraction are tightly linked, and they signal how PM-JAY can be systematically gamed if oversight is weak.[12][13][11][10]
Why PM-JAY is structurally vulnerable
- Information asymmetry is extreme: poor, often low‑literacy beneficiaries depend entirely on providers’ word about diagnosis and treatment, making it easy to oversell procedures such as stenting, hysterectomy, or ICU care.[1][10][5]
- Package-based payments create a menu of “prices” for each episode, incentivising upcoding (billing higher‑priced packages), procedure bundling, and unnecessary admissions when monitoring is weak; evidence of such practices has been documented in several states and schemes.[10][7][1]
- Provider markets are fragmented and weakly regulated; private hospitals can misreport bed strength, specialist availability, or accreditation status to get empanelled and then use PM-JAY volumes to cross‑subsidise other business lines.[2][1][10]
- Social and political pressures to show high utilization—“X crore treatments delivered”—can discourage aggressive fraud control at local levels because detected fraud statistically reduces reported coverage.[1][2]
Typology of PM-JAY frauds emerging
- Beneficiary‑side fraud: duplicate IDs, ineligible households, and transactions on cards of the deceased enabled by weak data validation and Aadhaar linking.[7][2][1]
- Provider‑side fraud:
- Phantom claims where no service is delivered but bills are submitted.[5][10][1]
- Upcoding and “package shopping” to maximize revenue per admission.[10][7][1]
- Unnecessary or harmful procedures (angioplasties, hysterectomies, cataracts, ICU stays) pushed on misinformed patients.[13][11][12][10]
- Circumventing rules that reserve certain procedures for public hospitals by misclassifying planned care as emergencies.[7][10]
- Collusive fraud: hospitals and insurance administrators, or hospitals and beneficiaries, sharing proceeds from inflated or fake claims while genuine claims from public facilities face denial or delay.[5][1][10]
Is PM-JAY the “next big low-hanging fruit”?
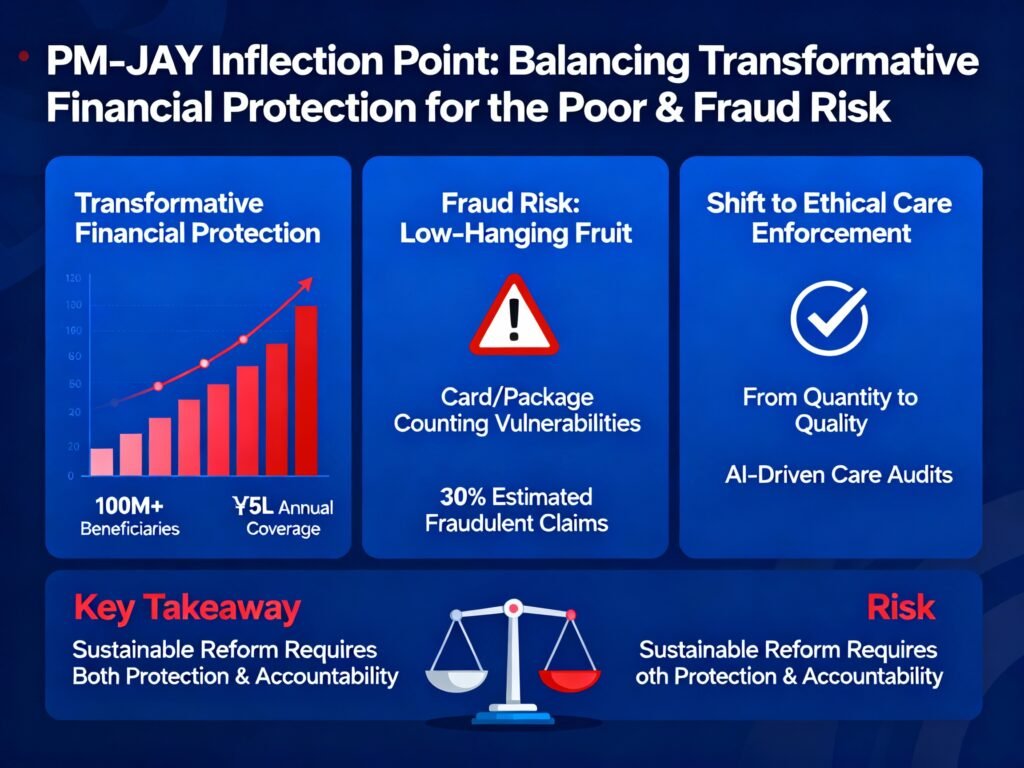
- Quantitatively, the number of hospitals flagged and crores recovered indicate that PM-JAY has already become a major target, but the scheme still finances only a small fraction of India’s total health spending, so fraud in self‑pay and private insurance remains larger in absolute terms.[6][3][2]
- Qualitatively, PM-JAY offers several “easy pickings” for unethical actors: predictable tariffs, vulnerable populations, and uneven state‑level enforcement, making it simpler to industrialise fraud than in fragmented retail insurance markets where private insurers can rapidly change contracts or deny suspect claims.[1][10][5]
- Unless regulation, medical audit capacity, and data analytics catch up, PM-JAY will continue to be viewed by some providers as a predictable, low‑risk revenue stream extracted through overtreatment and documentation games, rather than as a protective safety net for the poor.[9][2][10][1]
Policy and governance levers to change the trajectory
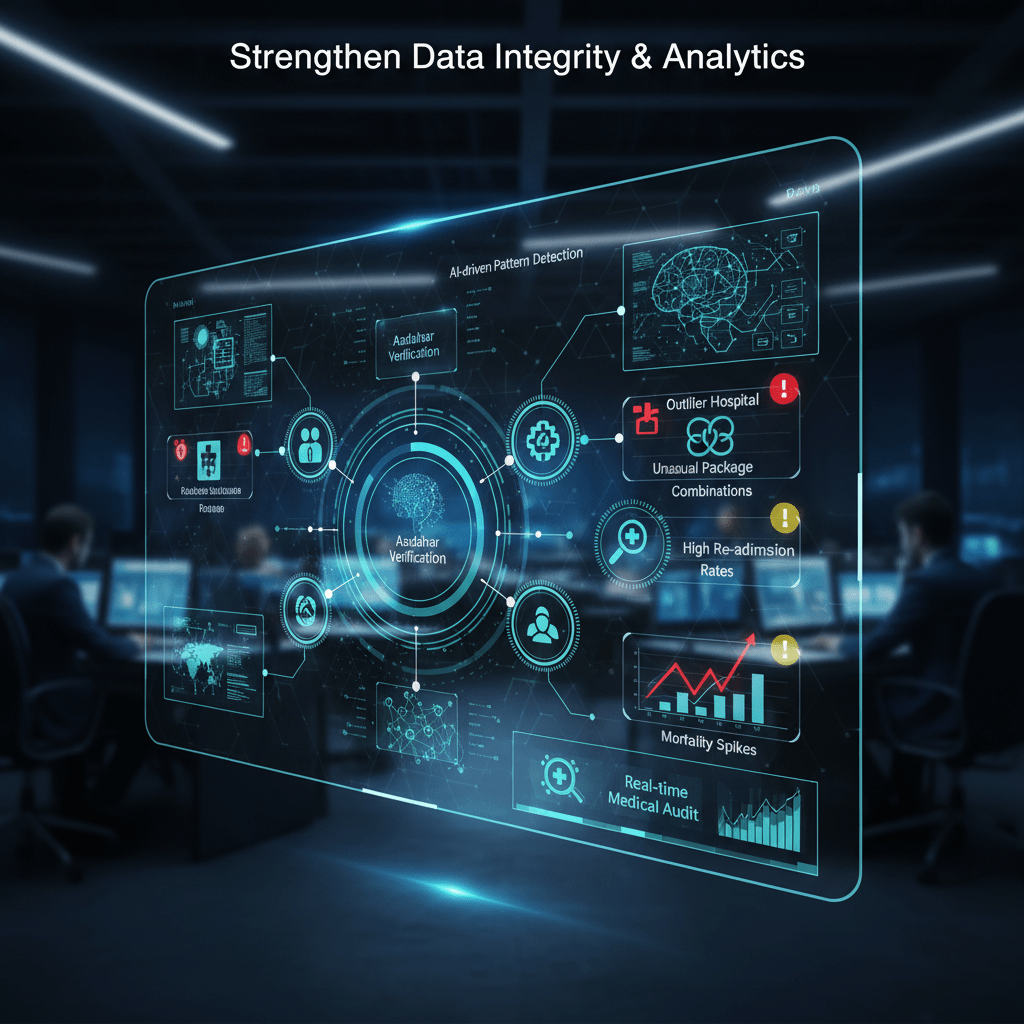
- Strengthen data integrity and analytics: fully integrate Aadhaar‑based verification, de‑duplicate beneficiaries, and deploy AI‑driven pattern detection to flag outlier hospitals, unusual package combinations, high re‑admission rates, and mortality spikes for real‑time medical audit.[9][2][7][1]
- Make clinical governance central: define state‑level medical audit cells with cardiology, surgery, and anaesthesia experts; mandate random pre‑authorization and post‑procedure review for high‑risk packages like angioplasty, hysterectomy, and neurosurgery.[9][10][1]
- Align incentives for public providers: ring‑fence PM-JAY reimbursements for infrastructure, staffing, and quality improvement in government hospitals so they compete less on volume and more on outcomes, reducing dependence on high‑risk private empanelment.[2][7][1]
- Raise the cost of fraud: ensure swift de‑empanelment, blacklisting, and criminal prosecution for documented fraud, and publish state‑wise “watchlists” of penalised hospitals to create reputational deterrence.[3][2][9]
- Empower beneficiaries and communities: invest in health literacy, transparent package information, and community monitoring so that patients and local leaders can question unexpected procedures or coerced admissions under the guise of “free” treatment.[10][5][1]
In that sense, PM-JAY is at an inflection point: the same characteristics that make it a transformative financial protection scheme also make it tempting “low‑hanging fruit” for fraud, and the balance will depend on how quickly India can move from counting cards issued and packages used to measuring—and enforcing—appropriate, ethical care.[3][2][1]

All Images are AI Generated for Illustration Only. E&OE
Sources
[1] CAG audit exposes multiple frauds in PMJAY https://iasscore.in/current-affairs/cag-audit-exposes-multiple-frauds-in-pmjay
[2] press release https://cag.gov.in/uploads/PressRelease/PR-PRESS-RELEASE-ON-REPORT-NO-11-ENGLISH-064d24b89c1a1e8-08708372.pdf
[3] Update on Strengthening of PM-JAY Implementation https://www.pib.gov.in/PressReleasePage.aspx?PRID=2157879
[4] Combating Fraud with Technology and Policy Reforms https://jpmsonline.com/article/download/787/
[5] Anti-Fraud Efforts in Government-Sponsored Health … https://documents1.worldbank.org/curated/en/946831555477597462/pdf/India-Case-Study-on-Institutional-Arrangement-for-Detecting-Fraud-in-Government-Health-Insurance-Program-Anti-Fraud-Efforts-in-Government-Sponsored-Health-Insurance-Schemes-in-Four-Indian-States.pdf
[6] Health Insurance Frauds in India – Types & Prevention 2025 https://joinditto.in/articles/health-insurance/health-insurance-frauds-in-india/
[7] Report https://cag.gov.in/uploads/download_audit_report/2023/Report-No.-11-of-2023_PA-on-PMJAY_English-PDF-A-064d22bab2b83b5.38721048.pdf
[8] Audit Reports | Comptroller and Auditor General of India https://cag.gov.in/en/audit-report/details/119060
[9] Measures taken to prevent misuse of AB-PMJAY Scheme https://www.mohfw.gov.in/?q=en%2Fpressrelease-195
[10] A typology framework for unethical medical practices under … https://ijme.in/articles/a-typology-framework-for-unethical-medical-practices-under-public-health-insurance-schemes-in-india-analysis-of-evidence-over-the-past-12-years/
[11] Khyati Hospital PMJAY Fraud: 15 patients move Gujarat HC for … https://medicaldialogues.in/news/health/hospital-diagnostics/khyati-hospital-pmjay-fraud-15-patients-move-gujarat-hc-for-separate-fir-registration-140822
[12] Khyati Hospital scandal: Doctors arrested in Gujarat for alleged … https://www.newindianexpress.com/nation/2024/Nov/14/khyati-hospital-scandal-doctors-arrested-in-gujarat-for-alleged-pmjay-fraud
[13] Gujarat PM-JAY Fraud: How Khyati Hospital used health camps to … https://economictimes.com/news/india/gujarat-pm-jay-fraud-how-khyati-hospital-used-health-camps-to-convince-patients-including-a-teen-for-unnecessary-angioplasty/articleshow/115804475.cms
[14] Jamnagar Hospital Faces Scrutiny for PMJAY Irregularities, 53 … https://english.dainikjagranmpcg.com/politics/jamnagar-hospital-faces-scrutiny-for-pmjay-irregularities-53-unnecessary-cardiac/article-8046
[15] Jamnagar hospital suspended from PMJAY https://health.economictimes.indiatimes.com/news/hospitals/unnecessary-heart-surgeries-jamnagar-hospital-suspended-from-pmjay/125327996
[16] Jamnagar hospital suspended from PMJAY | Ahmedabad News https://timesofindia.indiatimes.com/city/ahmedabad/unnecessary-heart-surgeries-jamnagar-hospital-suspended-from-pmjay/articleshow/125308693.cms
[17] Ahmedabad court rejects bail of Khyati hospital’s Milind Patel in … https://english.gujaratsamachar.com/news/gujarat/ahmedabad-court-rejects-bail-of-khyati-hospitals-milind-patel-in-pmjay-fraud-case
[18] Gujarat PMJAY racket scam: Khyati multispeciality hospital chairman … https://indianexpress.com/article/cities/ahmedabad/gujarat-pmjay-racket-scam-khyati-multispeciality-hospital-chairman-arrested-9785692/
[19] A web of deceit surrounding the Ayushman Bharat Pradhan Mantri … https://www.facebook.com/MirrorNow/posts/a-web-of-deceit-surrounding-the-ayushman-bharat-pradhan-mantri-jan-arogya-yojana/915919447331413/
[20] PM-JAY ‘Scam’ In Gujarat; Ahmedabad Hospital Shocker … – YouTube https://www.youtube.com/watch?v=GrUcaYPSje4
[21] Health Insurance Frauds in India https://www.policyx.com/health-insurance/articles/health-insurance-frauds-in-india/