When an eminent cardiologist like Dr. Sunil Chandy—former Director at CMC Vellore—calls out the “medical colonialism and exploitation that has gripped Indian healthcare,” it stops you cold.
His words grab you by the collar, forcing a reckoning with a system that boasts world-class care for medical tourists while bankrupting its own citizens at the hospital gate.
This blog peels back the layers of that illusion—cyber-coolies in scrubs, public pain fueling private gain, and a desperate need for sovereign health reforms—demanding India choose between proud citizens and well-trained servants.
Indian healthcare is in danger of becoming the gleaming back office of a global medical empire, while its own citizens are bankrupted at the hospital gate. This is not sovereignty; it is a high‑tech replay of colonial extraction dressed up as “Heal in India” and “world‑class” care.

The illusion of world‑class pride
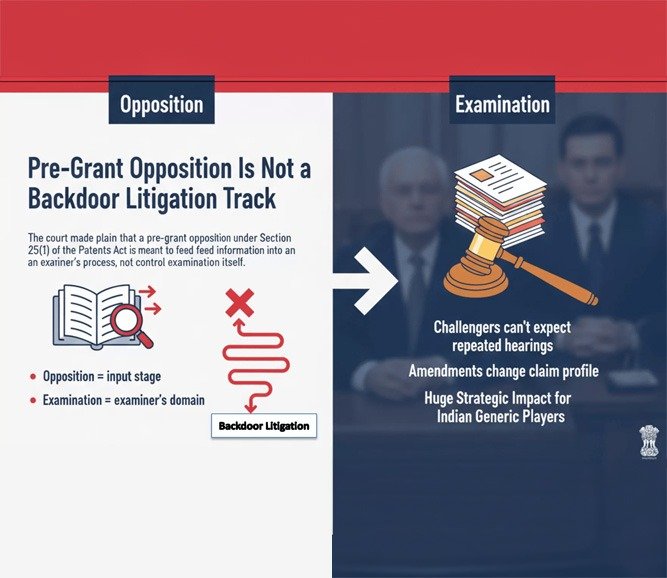
Corporate hospitals and policymakers like to boast that a cardiac surgery in India costs a fraction of what it does in the US or UK. They celebrate the medical tourists who fly in for “affordable” bypasses, robotic surgeries, and organ transplants. But the benchmark in this story is not the Indian worker earning in rupees; it is the dollar‑paying foreigner or the Indian elite with an international credit card.
This is the central sleight of hand: India is told to be proud that its surgeons operate at “1/10th the price” of Western hospitals, even as ordinary Indians struggle to afford a single night in an ICU. The system celebrates arbitrage—cheap Indian labour, cheap Indian infrastructure, cheap Indian risk—while exporting value to global insurers, brokers, and medical tourists.
http://linkedin.com/in/sunil-chandy-92b97430
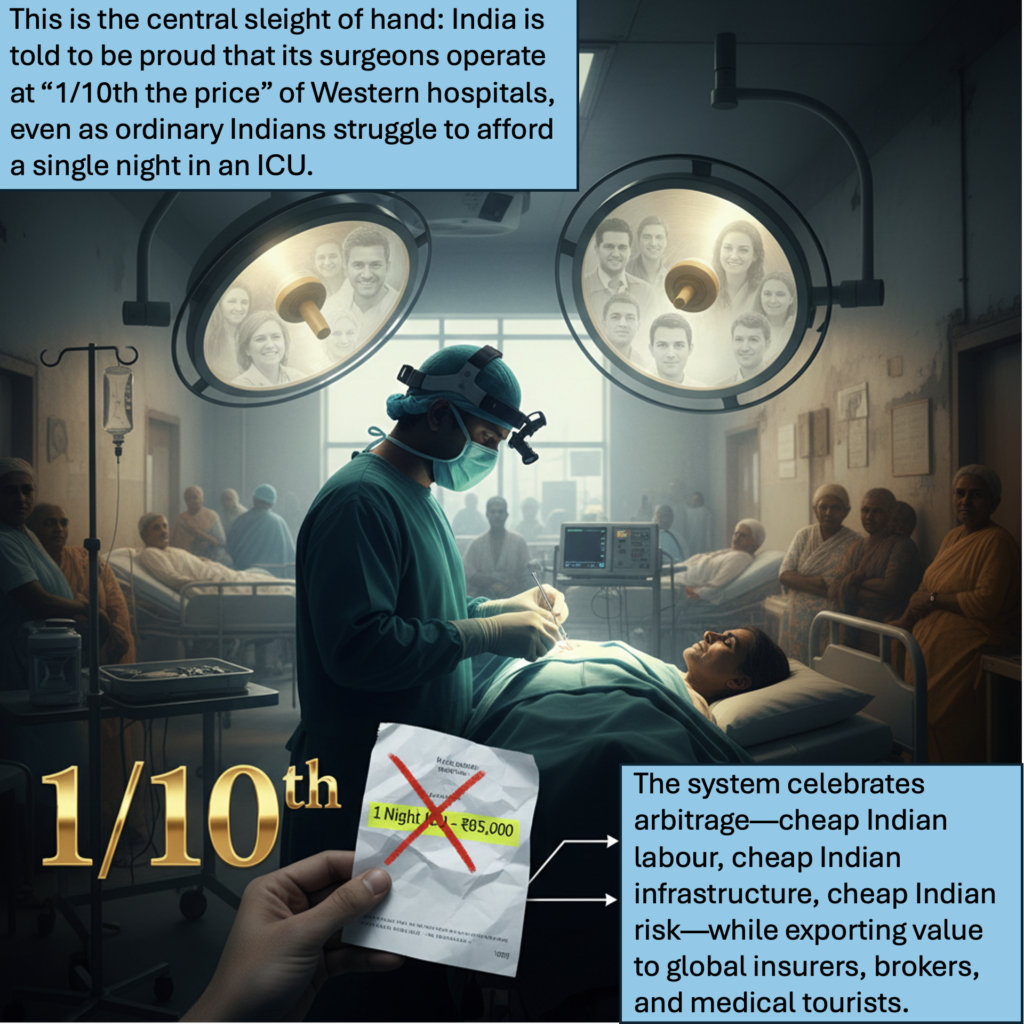
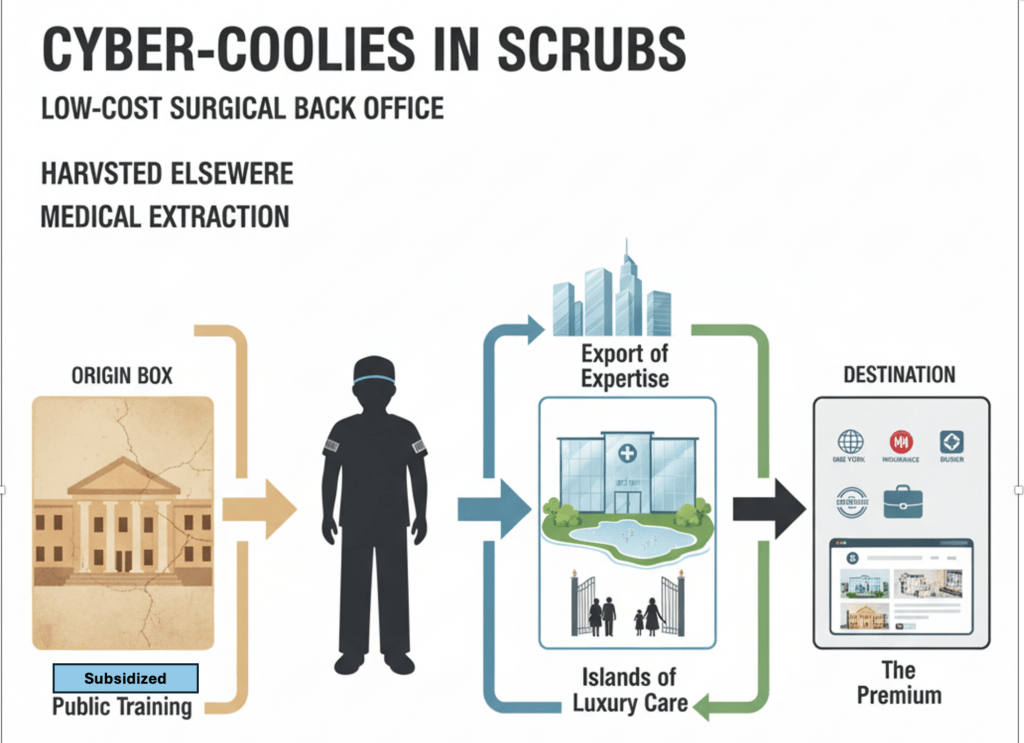
Cyber‑coolies in scrubs
For three decades, India has been sold the dream of “moving up the value chain,” away from being the world’s back office and IT sweatshop. In healthcare, the opposite is happening. The country is steadily positioning itself as the low‑cost surgical back office of the Global North.
Indian clinicians are world‑class, but they are trapped in a script not of their making. The best doctors are trained in public institutions subsidised by Indian taxpayers, then encouraged to migrate to the UK, US, and Gulf or to join corporates that chase foreign patients. The value of their expertise is harvested elsewhere, or within islands of luxury care inaccessible to their fellow citizens. India supplies the skills; others write the rules and take the premium. That is not partnership; it is a modern, white‑gloved form of medical colonialism.
Public pain, private gain
Look at the architecture of the system:
- Public funds build roads, airports, and urban infrastructure that conveniently funnel patients into private hospital clusters.
- State governments hand out land, tax breaks, and import duty waivers in the name of “health sector growth.”
- Medical colleges and government hospitals shoulder the cost of training the workforce.
And yet, when an ordinary Indian family faces a medical emergency, they meet an unforgiving paywall. Insurance is patchy, exclusions abound, and cashless promises vanish in the fine print. A single hospitalisation can annihilate years of savings, push a household below the poverty line, or trap them in lifelong debt. This is a system where public risk and public money underpin private profit, while the public’s own health security remains an afterthought.

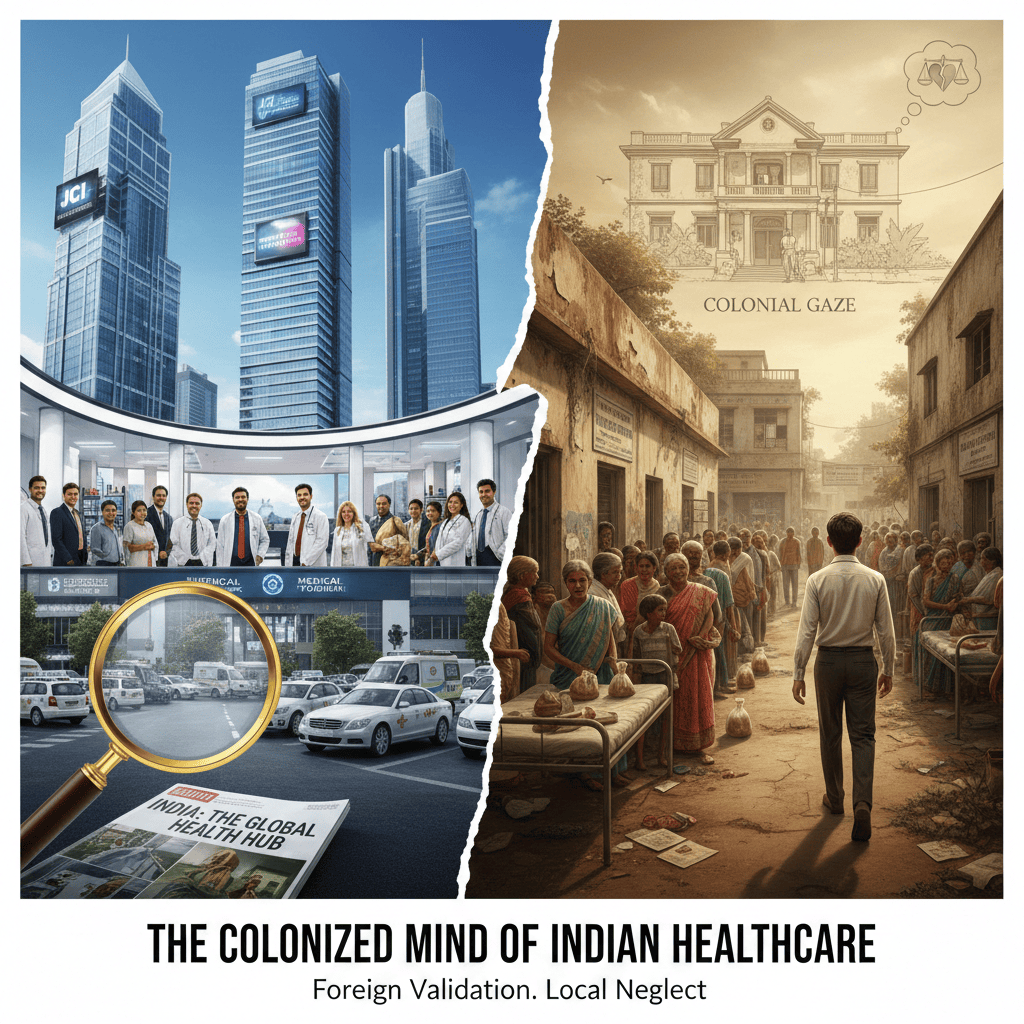
The colonised mind of Indian healthcare
The tragedy is not only economic; it is psychological. Indian healthcare continues to measure its worth in foreign validation:
- International accreditations become the gold standard, even when they have little to do with what Indian patients actually need.
- English‑speaking specialists in glass towers are revered, while district hospitals and primary centres are starved of respect, talent, and funds.
- Success is redefined as “attracting global patients” instead of ensuring that no Indian has to sell land, jewellery, or their children’s education for treatment.
The colonial gaze has simply moved from the Viceroy’s bungalow to the global rating agency and the medical tourism brochure. We have internalised a hierarchy where serving the first‑world patient is prestigious, while serving the local poor is charity. That mentality is the deepest stain of medical colonialism.
A sovereign health system or a service vendor?
India cannot claim to be a truly sovereign nation while its health system behaves like an outsourced service centre for richer economies. Sovereignty is not a flag and an anthem; it is the ability to protect the lives and dignity of one’s own people before catering to external demand.
A sovereign health system would:
- Treat catastrophic health expenditure as an unacceptable policy failure, not a regrettable side‑effect of “market efficiency.”
- Put public primary care, district hospitals, and emergency services at the centre, with corporate hospitals playing a regulated, clearly bounded role.
- Demand reciprocity: if global capital and foreign patients benefit from India’s low costs and skilled workforce, then the cross‑subsidy to Indian patients and public infrastructure must be explicit, measurable, and enforceable.
- Invest in Indian clinical research and guideline development that answers Indian questions—TB, sepsis, road trauma, maternal mortality—rather than simply importing Western protocols and devices.
Anything less is a continuation of dependency economics in a white coat.

What breaking with colonial legacies really means
If India wishes to stop being the world’s cut‑price operating theatre, it needs a deliberate, politically uncomfortable reset:
- Rebuild the public spine: Massive, sustained investment in primary care, diagnostics, and district‑level hospitals, with pay and working conditions that attract top talent—so that the default choice for most citizens is a strong public system, not desperation in the private market.
- Chain the corporate behemoth: Transparent price regulation for common procedures, mandatory reporting of outcomes and complications, and strict caps on balance‑billing. Public concessions to hospitals must be conditional on demonstrable free or subsidised care for Indian patients, not vague CSR.
- Fix insurance, don’t expand illusions: Health insurance must stop being a subsidy pipeline to corporates. Standardised packages, hard ceilings on non‑medical charges, and swift grievance redressal are the minimum. Protection from ruin, not bed occupancy, should be the key performance indicator.
- Reverse the brain drain logic: Tie publicly funded specialist education to a period of service in the public system or tier‑2/3 cities, with real career progression and research opportunities. Make it prestigious to run a top‑notch district hospital, not only a metro flagship.
- Reclaim the narrative: Indian professional bodies, journals, and educators must define quality in terms of population health and equity, not just technology and hotel‑like amenities. “World‑class” should mean that a poor patient in a small town receives timely, competent care without fear of financial annihilation.
A call to India’s healthcare community
The industry cannot hide forever behind the language of “market forces” and “global competitiveness.” Every clinician, manager, policymaker, and pharma leader must decide which India they are building:
- An India that trains doctors with public money so they can serve medical tourists and foreign health systems; or
- An India that uses its formidable clinical talent and frugal innovation to guarantee that no citizen is left untreated or impoverished.
The first path leads to polished servitude—a health system of cyber‑coolies in scrubs, optimising spreadsheets and clinical pathways for overseas value. The second path is harder, less glamorous, and politically fraught, but it is the only one worthy of a republic that calls itself sovereign.
If we do not consciously break with the colonial logic of extraction and external validation, India will remain what it is rapidly becoming: a low‑cost surgical back‑office for the rich world, while its own people bleed at the billing counter. The question for Indian healthcare is brutally simple—do we want to be a nation of proud citizens, or a nation of well‑trained servants?

Sources:
Priya Shetty, “Medical tourism booms in India, but at what cost?”, The Lancet, 2010.[thelancet]
• “Healthcare Apartheid in India: A Legacy of Colonialism”, rapid response, BMJ, 2023.[bmj]
• “Impoverishing effects of out‑of‑pocket healthcare expenditures in India”, Journal of Education and Health Promotion, 2022.[pmc.ncbi.nlm.nih +1]
• “Do hospitalizations push households into poverty in India: evidence from national data”, F1000Research, 2024.[f1000research +1]
• “How Does the Largely Unregulated Private Health Sector Impact the Indian Poor?”, Indian Journal of Public Administration (SAGE), 2019.[journals.sagepub]
• Thirusha Naidu, “Coloniality lives on through medical education”, BMJ, 2023 (for broader coloniality arguments).[bmj]