India’s health map is splitting into two distinct opportunity zones for pharma: states that are putting health near the top of their budget priorities, and those that still lean heavily on out‑of‑pocket spending and thin public systems. This divergence is no longer just a policy curiosity; it is becoming a core commercial variable that should shape portfolio strategy, go‑to‑market design, and marketing investments for every serious Indian pharma player.
The new state health economy
Over the last decade, government health expenditure has risen both as a share of GDP and of total health spending, with states now financing the bulk of public health outlays. Yet there are sharp differences in commitment: some states allocate upwards of 6–7% of their budgets to health and actively expand insurance, free‑drug schemes and public infrastructure, while others remain closer to 4–5%, leaving households to bridge the gap through out‑of‑pocket payments. Medicines continue to form the largest single component of personal health spending, which keeps drug prices, procurement efficiency and pharma margins squarely in the political spotlight.[1][2][3][4][5]
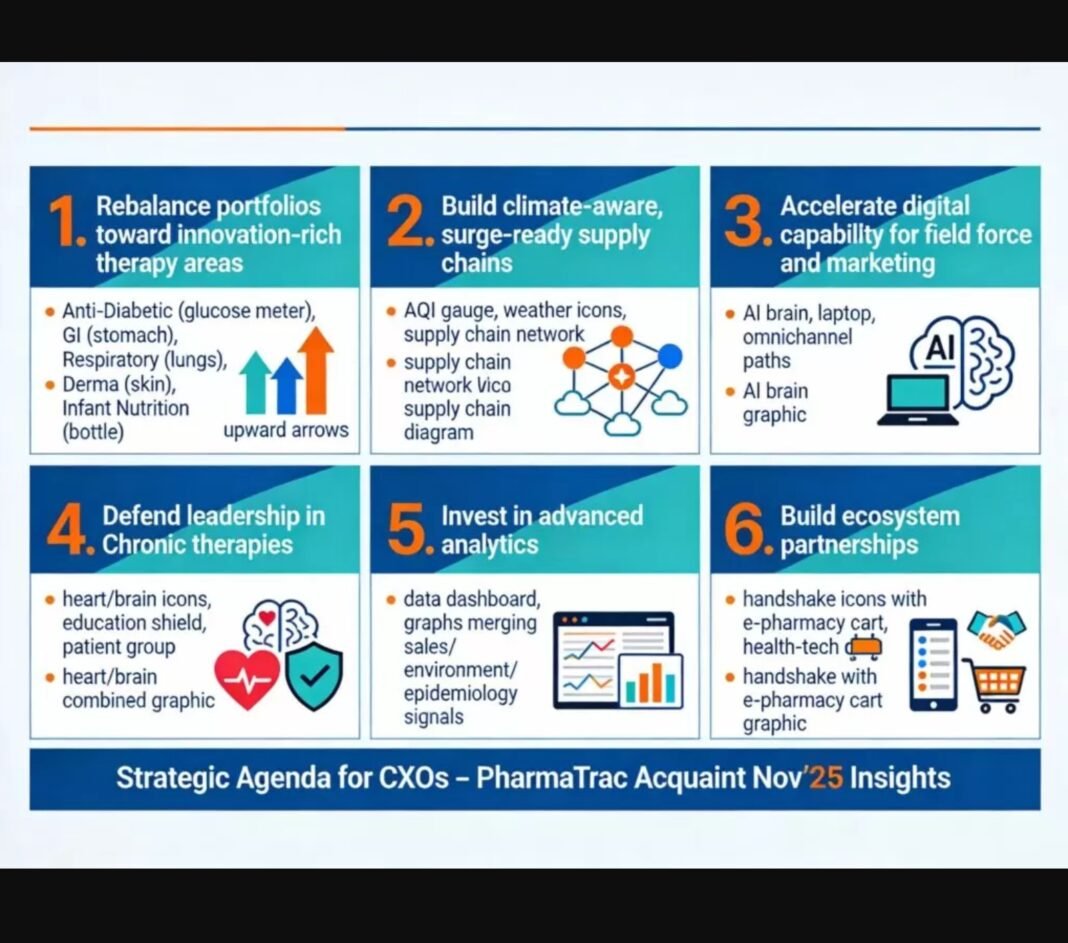
For pharma C‑suites, this means national strategies that ignore state‑wise fiscal capacity and policy ambition are increasingly obsolete. The winners will be companies that segment India not just by therapy or geography, but by “health‑spend archetype” and then calibrate offers, evidence and engagement models accordingly.
1. High‑spend states: build health‑system partnerships

In higher‑spend states—those pushing health towards or beyond 6% of their total budget—the state is evolving from a passive payer to an active architect of care pathways. These states are expanding insurance coverage, strengthening primary care, and scaling up free‑medicine schemes, which concentrates volumes in public procurement channels and formal formularies rather than fragmented retail scripts.[2][3][4][7]
Actionable strategies for C‑suite leaders:
- Create state‑specific market‑access pods
- Establish cross‑functional teams (medical, HEOR, policy, sales) dedicated to priority high‑spend states, with clear P&L responsibility.
- Map procurement agencies, formulary committees, program directors and digital‑health initiatives, and maintain a live “health‑system CRM” with decision timelines and data needs.
- Shift from brand selling to value propositions
- Develop health‑economic dossiers and budget‑impact models that demonstrate how your therapies reduce hospitalizations, complications or productivity loss across large covered populations.
- Offer integrated solutions: drug plus diagnostics, adherence tools, tele‑consult support, and training for public‑sector clinicians and field workers—positioning the company as a partner in achieving state health targets, not just a vendor.
- Pilot innovative contracting and digital programs
- Use high‑spend states as sandboxes for outcomes‑linked contracts, risk‑sharing pilots and digital disease‑management programs in NCDs, maternal‑child health, and mental health.
- Co‑design public‑education and screening campaigns with health departments, embedding your brands into state‑led care pathways in a compliant, evidence‑based manner.
2. Low‑spend states: compete on access and affordability

In lower‑spend states, limited public budgets mean households still shoulder most healthcare costs and private providers dominate service delivery. Here, the addressable market is driven less by government tenders and more by consumers’ ability to pay, informal provider networks and fragmented retail channels, especially beyond metros and tier‑1 cities.[3][5][7][8]
Actionable strategies for C‑suite leaders:
- Anchor on affordable portfolios and tier‑2/3 coverage
- Prioritise high‑volume, affordability‑focused branded generics, basic chronic therapies, and OTC/consumer‑health lines that match local purchasing power.
- Build deep distribution in tier‑2/3 towns and rural belts through strong trade partnerships, incentive structures and localised brand education for chemists and informal providers.
- Design financial‑protection‑oriented patient programs
- Introduce therapy kits, subscription dosing, and bundled pricing that smoothen cash outflows for chronic patients.
- Use teleconsultation tie‑ups and low‑cost diagnostic partners to reduce the “total cost of care” around your drug, not just the pill price.
- Shape emerging policy before it scales
- Engage constructively with state health departments, professional bodies and development partners to supply data on disease burden, treatment gaps and cost‑effective protocols.
- Aim to influence the first iterations of essential‑drug lists, reimbursement rules and standard‑treatment guidelines so that, as budgets eventually rise, your molecules are already embedded in policy.
3. Recalibrating marketing and access investments

Indian pharma already spends a higher share of revenue on marketing and promotion than many other healthcare segments, with estimates clustering around 18–21%, compared to 7–10% for healthcare overall. Historically, much of this spend has gone into doctor‑centric promotion and trade schemes, with limited transparency on what portion actually shifts access or outcomes. As state health budgets diverge, a more surgical allocation of marketing rupees becomes essential.[7][9][10][11]
Actionable strategies for C‑suite leaders:
- Split marketing into two explicit buckets
- Create a dedicated “Institutional Access and Policy” budget focused on health‑system engagement: tender participation, HEOR, policy advocacy, public‑health campaigns and digital programs aligned with government schemes.
- Maintain a separate “Private‑Market Growth” budget for HCP engagement, consumer advertising, and trade activation in markets where out‑of‑pocket spending dominates.
- Weight investments by state archetype and maturity
- In high‑spend states, tilt more budget towards institutional access: evidence generation, outcome registries, training partnerships and omnichannel engagement of public‑sector HCPs.
- In low‑spend states, focus spend on retail pull (doctor and chemist education, consumer awareness, rural activation) and scalable digital tools that cut CAC while widening reach.
- Upgrade governance, data and capability
- Institute strong compliance frameworks around public‑sector engagement and tendering to mitigate ethical and reputational risk.
- Build analytics capability to track state‑wise health allocation trends, scheme expansion, therapy adoption and campaign ROI, allowing dynamic re‑allocation of spend each budget cycle.
- Retrain field forces—from “product detailers” to “solution consultants”—who can discuss protocols, outcomes and system pain‑points with administrators as comfortably as they discuss brands with clinicians.
For Indian pharma, the next decade will not be defined only by which therapies win, but by which companies master the art of state‑specific strategy. Those that learn to partner deeply with high‑spend states, compete smartly and ethically in low‑spend markets, and treat marketing budgets as levers of access and outcomes—not just visibility—will be the ones that shape, and benefit from, India’s evolving health‑spend landscape.[10][1][2][3]
Sources
- GOVERNMENT OF INDIA MINISTRY OF HEALTH & FAMILY WELFARE
- National Health Accounts Estimates for India
- State-wise Healthcare Spending in India for 2025
- Mapping Budget Priorities for the Health Sector of Select States in India
- Medicines take lion’s share of personal healthcare spending
- A cross-sectional analysis from the state of Odisha, India
- Healthcare Market Landscape in India
- Government Initiatives to Healthcare Expenditure in India
- Healthcare Advertising in India 2026: Trends, Media Mix & Case Studies
- Customer Acquisition Cost (CAC) & Indian Pharma | MedicinMan
- Pharma Marketing Trends 2025: Digital Transformation & Patient Engagement